TORONTO - Shannon Pethick thought cervical cancer would be in Canada's rear-view by now.
"It hurts my heart because we should be past this," she said from her home in Saskatoon, reflecting on her diagnosis 15 years ago, at age 32.
But the latest ║├╔źtv Cancer Statistics report says the country may not reach its goal of eliminating cervical cancer by 2040.
Data published by the ║├╔źtv Cancer Statistics Advisory Committee shows a ÔÇťconcerning plateauÔÇŁ of cervical cancer rates, signalling Canada is moving in the wrong direction.
The World Health Organization set a global goal in 2018 of virtually eliminating this type of cancer, which is caused by the human papilloma virus, a common sexually transmitted infection, to fewer than four cases diagnosed per 100,000 females.
Canada was making progress for decades as rates steadily declined between 1984 and 2005, but since then the trend has fluctuated.
The report says 430 people in Canada are expected to die from cervical cancer in 2025. While that accounts for a small portion of the 87,400 expected deaths due to cancer in the country this year, all of them are potentially preventable. Unlike many other cancers, there's a vaccine to prevent this one.
"There's no reason for there to be over 400 people dying this year from cervical cancer," Pethick said.
The "what ifs" still linger for her. What if she had gone for a routine Pap test cervical cancer screening, instead of putting it off for seven years.
She underwent two months of radiation five days a week, chemotherapy on Fridays, and five sessions of internal radiation, and she is now cancer-free.
"Doing all of this and getting this thing out of my body also meant that I was never going to be able to have kids," she said.
The cancer was growing fast and doctors said taking time to freeze her eggs could have been harmful.
"I still struggle with that," Pethick said as she lifted her glasses to stop tears from falling down her cheeks.
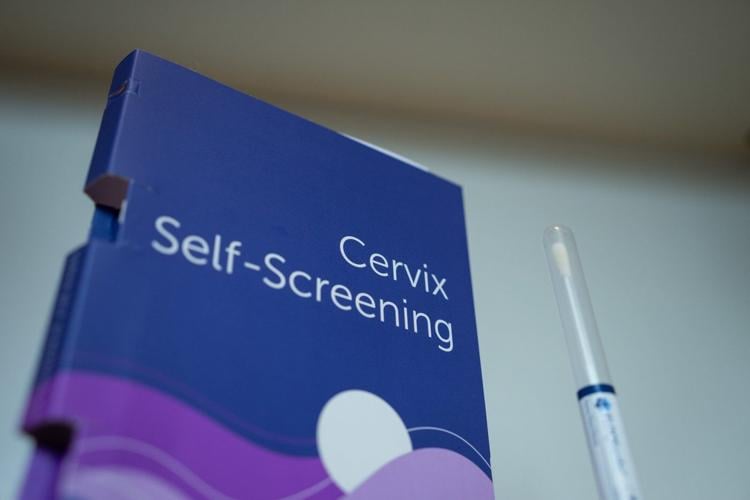
She said the invasive nature of a Pap, which involves inserting a speculum into a patientÔÇÖs vagina to swab their cervix, deterred her from the exam. If an HPV self-testing kit was an option at the time, she says she would have tested earlier.
Self-testing is used in British Columbia, and considered just as accurate as tests collected by a health provider. Similar plans are underway in New Brunswick, Nova Scotia and Prince Edward Island.
The ║├╔źtv Cancer Society's director of surveillance Jennifer Gillis says Canada is not where it had hoped to be likely due to lower HPV vaccination rates, a decline in the rate of people getting screened, and gaps in followup care.
Gillis says there are so many tools available to change the current trajectory, such as switching from the Pap test to the HPV test.
She also says the HPV vaccine should be free for those who missed getting it in school, as the cost ÔÇö three doses at $215 per shot ÔÇö is a barrier.
Canada's plan to eliminate cervical cancer included a target of fully immunizing 90 per cent of 17-year-olds with the HPV vaccine by 2025.
The ║├╔źtv Partnership Against Cancer says only three provinces, Prince Edward Island, Newfoundland and Labrador, and Quebec, are reporting rates above 80 per cent.
The Federation of Medical Women of Canada said in a paper last year that fewer than 20 per cent of ║├╔źtvs have had the HPV vaccine.
Dr. Milena Forte, a member of the federation and family doctor in Toronto, says the HPV vaccine has always had lower uptake than other routine vaccines.
"There is still this association or misinformation around the fact that by providing this vaccine you're somehow condoning any sexual behaviour," Forte said.
"We have a free way to decrease rates of cervical cancer," she said. "Everybody should be lining up for this."
This report by ║├╔źtvwas first published Nov. 17, 2025.
║├╔źtv Press health coverage receives support through a partnership with the ║├╔źtv Medical Association. CP is solely responsible for this content.
Note to readers:This is a corrected story. A previous version misspelled Shannon Pethick's surname in one instance.